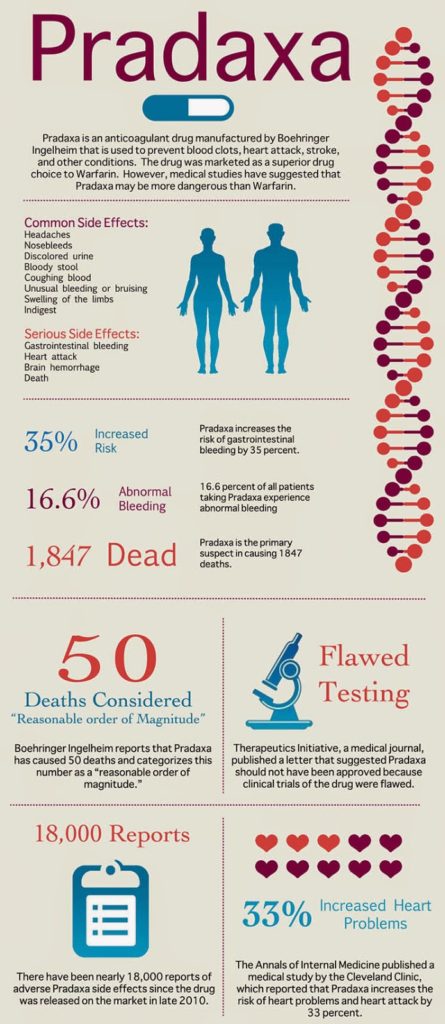
Boehringer’s anti-clotting drug Pradaxa is marketed as better and safer than warfarin, the generic and much cheaper alternative. The ads specifically mention that no frequent blood tests are needed to monitor the safety and effectiveness of Pradaxa, whereas such tests are necessary for warfarin.
This makes it easier to sell Pradaxa to cardiologists and family practitioners who can pass on these obvious safety advantages to patients who need to carefully weigh benefits vs. risks of these powerful drugs.
But this task is made much more difficult when there are two post-marketing approval safety studies that come to two different conclusions. Considering that news of the studies has been released on the same day (today), the stage is set for battling it out in public.
One study of Medicare patients — by the FDA — was published online in Circulation on October 30, 2014. A press release dated today (November 3, 2014; here) claimed that it “further reinforces the favorable benefit/risk profile of PRADAXA.”
Another, independent study of Medicare patients, titled “Dabigatran Associated with Higher Incidence of Major Bleeding vs. Warfarin,” was published online November 3, 2014 in JAMA Internal Medicine (and embargoed until 3 pm Central). That study claimed that the “incidence of major bleeding was 9 percent for the dabigatran (Pradaxa) group and 5.9 percent for the warfarin group.” The takeaway from that study: “Prescribe Blood Thinner Pradaxa With Caution.”
How do two different studies seemingly reach two different conclusions based on the same population? And which study will Boehringer (BI) distribute to docs via its sales reps? See below for my take on that.
Update (5-NOV-2014): When I originally posted this article, I also should have asked: “Which study would BI highlight in a press release to inform the media, physicians, patients and its more than 40K Twitter followers?” And what would a “Patient-Centric” approach dictate? See the end of this post for my views on that.
First, let’s talk about the differences between these studies.
The authors of the JAMA Internal Medicine study note that the FDA failed in another study (RELY) to adjust for differences in patient characteristics, which would bias the results.
“We found opposite results comparedwith the FDA’s investigation, which did not adjust for differences in patient characteristics between the treatment groups,” said the authors. “Dabigatran and warfarin users are very different in several factors that directly affect the risk of bleeding, and failing to adjust would bias the results.” Their study adjusted the data for these differences in population.
The FDA study reported in Circulation also does not adjust the data based on patient risk tolerance. It says it is “based on data from elderly patients older than 65 years enrolled in Medicare who started therapy with PRADAXA or warfarin between October 2010 and December 2012. Each group comprised 67,207 patients.” NOTE: The JAMA study results were based on 8,102 warfarin users versus 1,302 Pradaxa users.
Although the press release title (“FDA Study of Medicare Patients Reaffirms Safety and Efficacy Profile of Pradaxa® (dabigatran etexilate mesylate) for NVAF”) doesn’t mention it, this study found that Pradaxa exhibited “a significantly increased risk of major gastrointestinal hemorrhage” than does warfarin. Hmmm…
These studies obviously convey two conflicting safety messages, which are difficult to reconcile by non-statisticians. I’m sure it is beyond the capabilities of most Medicare patients to determine which study is best suited to their needs. These patients, therefore, depend upon their physicians to help them weigh the benefits vs. the risks.
And which study will reign supreme with physicians? It all depends on their sources of information. Pharma companies — including BI — are major sources of information about drugs for many physicians. And an important method pharma employs to get this information to physicians is through the distribution of reprints from peer-reviewed journals such as JAMA Internal Medicine and Circulation.
BI, of course, will distribute reprints to its physician customers according to the new FDA guidelines, which specifically address the distribution of reprints regarding “new risk information.” That guidance states:
“FDA does not intend to object to the distribution of new risk information that rebuts, mitigates, or refines risk information in the approved labeling, and is distributed by a firm in the form of a reprint or digital copy of a published study” if the study or analysis meet specific conditions (read about the conditions here).
FDA’s rules do not require BI to distribute reprints of BOTH studies mentioned here. So, it’s perfectly “legal” for BI to distribute only the Circulation reprint, which, of course, would bias the advice given to patients by physicians who only see that data.
Hopefully, BI will take a more balanced, educational approach such hosting a TweetChat to answer the questions from physicians about how these two studies impact the benefit vs. risk profile of Pradaxa. BI, after all, is a master of the TweetChat focused on physicians and the media (see “How to Host a Successful Pharma TweetChat“).
Oh, I forgot! FDA regulations regarding Twitter probably make that impossible (see “FDA Sets Up a Roadblock for Branded Rx Promotional Tweets“).
UPDATE (5-NOV-2014): BI published a press release on NewsWire about the Circulation study and on its website (see “FDA Medicare study in 134,000 atrial fibrillation patients confirms positive safety profile and effectiveness of Pradaxa® in general practice“). It also posted the following tweets via its German and US Twitter accounts:
BI did NOT, however, publish anything about the JAMA study. Consequently, there were many more tweets linking to BI’s press release and many more articles in the media (such as this MM&M piece) that focused exclusively on the Circulation study results.
The message from the JAMA study — i.e., “Prescribe Blood Thinner Pradaxa With Caution” — is lost among all the press and social media chatter generated by BI about the Circulation study. If BI wants to be more “Patient-Centric” — which I am sure its does — I think it should take a leading role in conveying this message to physicians and patients through its influential “word-of-mouth” channels rather focusing exclusively on the benefit side of the equation.








![6 Digital Tools at the Center of Healthcare Digitalization [INFOGRAPHIC]](http://ec2-54-175-84-28.compute-1.amazonaws.com/pharma-mkting.com/wp-content/uploads/2021/04/6DigitalTools_600px-100x70.jpg)




