Successful promotional medical education (Promo MedEd) programs engage, enlighten, and ultimately shift the behaviors of healthcare providers. These programs are successful because they are part of a strategic plan with clear, measurable educational and behavioral objectives. This coordinated series of face-to-face and nonpersonal activities is designed to move providers into action.
Make every interaction matter
As medical information proliferates, marketing channels multiply, and traditional outreach through sales representatives declines, it is difficult to catch and hold provider attention. That’s why it’s critical to make every interaction matter.
Performance-Driven Medical Education™ (PDME) is an integrated approach designed to elevate brand value. It focuses on education first, then on harmonizing medical education and promotional communications. It unites science, storytelling, behavioral science, and neuromarketing to amplify the power of your brand. PDME is an education-first idea that applies marketing principles to medical education and vice versa.
Here are 5 ways you can enhance the performance of your medical education programs. When these fundamentals are incorporated into medical education programs, their effectiveness improves.
1. Employ storytelling
Engage the human, not just the physician. Humans have a natural affinity for stories because they trigger emotional responses while using facts and a narrative to communicate something important. Studies show that narratives, which are often processed more efficiently, are associated with increased recall and ease of comprehension.
Everyone has emotions…even physicians.
If you want to influence a practitioner, provide an experience that connects emotionally. Stories set the stage and show a problem as a thread of connected events, making it easier to visualize and feel the resolution. Delivering the credible science behind a product in a story with a clear, connected arc can engage physicians, improve understanding, and inspire action more effectively.
2. Evaluate visual effectiveness
Slide decks remain our industry’s principle means of sharing information with providers. Although new, immersive technologies are exciting and are gaining traction, like it or not, the slide deck remains the go-to tool.
How do you know if your key slides are optimized for visual effectiveness? A practical approach to ensure that your content is optimized for efficient and effective absorption is to eliminate visual noise—remove elements that distract from your primary message.
Artificial intelligence and predictive modeling tools can simulate a viewer’s attention and predict the content a person is most likely to absorb or ignore in a presentation. You can simulate viewing conditions, pre-test materials, and modify the design for optimal viewing with high predictive accuracy.
Ensuring optimal visual delivery can engage and focus the viewer’s attention, enhance the presenter’s narrative, and provide the best opportunity to convey your perspective. Visual effectiveness is an overlooked, but important nuance when battling for physician attention.
3. Engage the senses
Healthcare providers have different ways of accumulating knowledge. By understanding learning styles, you can enhance the effectiveness of your medical education programs.
Like all adult learners, doctors and other providers learn via one or more of the 3 primary learning styles: visual, auditory, and kinesthetic. Visual learners need to see pictures and graphs to absorb information. Auditory learners need to hear the information. Kinesthetic learners need to engage in an activity to grasp a concept.
Remember, a mix of the 3 learning styles is how adults learn best. Ensure that your content is delivered via a multisensory approach to effectively convey educational content. From emails to videos, a wide range of engagement tactics can achieve this goal. Immersive technologies such as augmented reality and virtual reality combine multisensory learning in one experience and are useful approaches when utilized appropriately.
4. Enhance recall
You’ve got a strong medical education story to tell, your slides are visually optimized, your content is ready to be delivered via a multisensory approach. All you need to do is hit go, right? Not exactly.
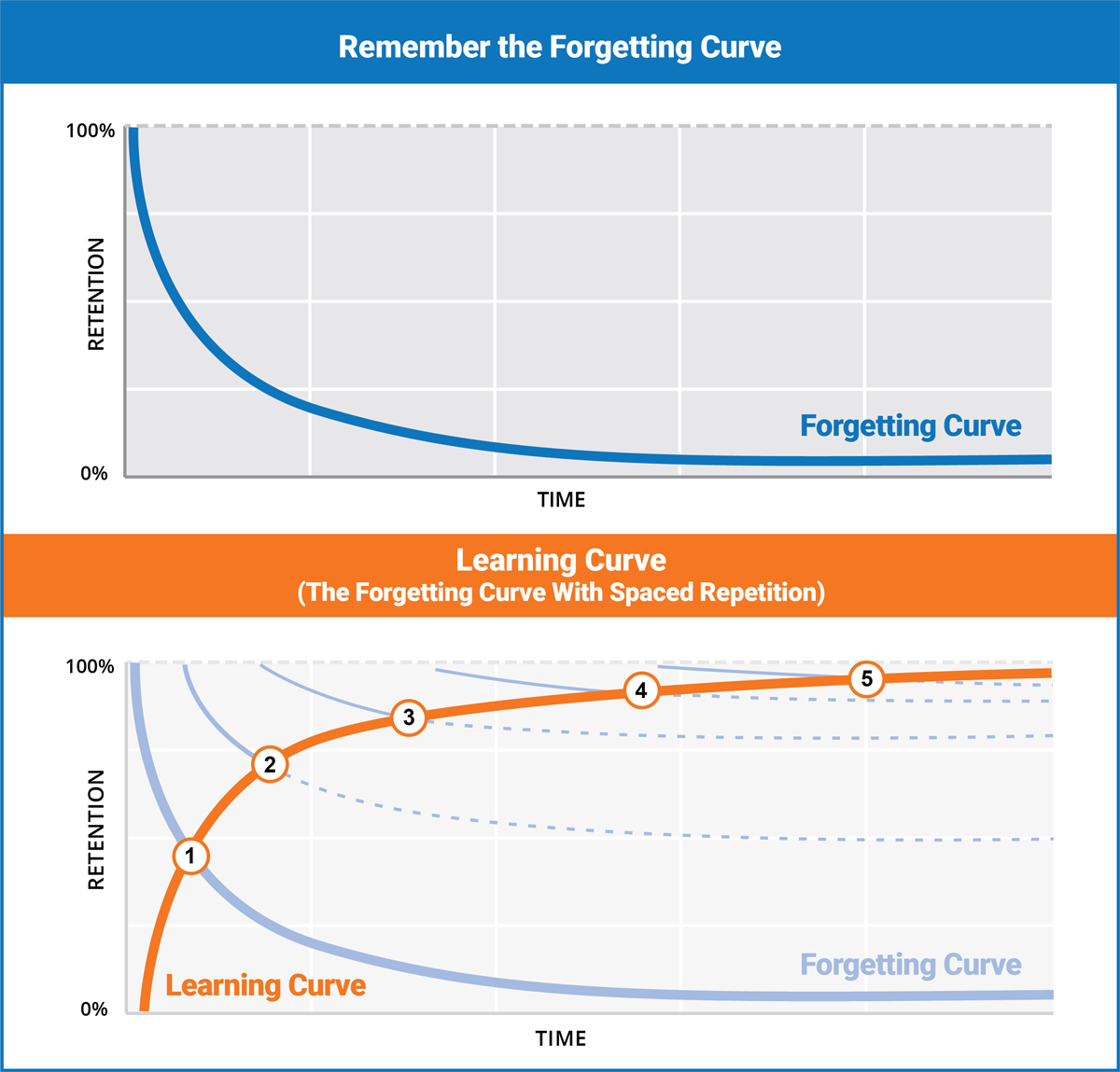
Remember the forgetting curve
The forgetting curve demonstrates how information is lost over a period of time when there is no attempt to retain it. Consider the following: People (physicians) will forget an average of 50% of the information you present within 1 hour. They will forget approximately 70% of your content within 24 hours and 90% within 1 week!
Consider how much money and effort is put into your programs, only to have the content be forgotten. The forgetting curve makes it clear: One-and-done medical education programs don’t work.
Combat the forgetting curve with spaced repetition of the new content. Spaced repetition is a learning technique that is based on reviewing information at gradually increasing intervals. It’s a useful strategy for long-term knowledge acquisition.
A robust follow-up plan using spaced repetition principles is essential to the performance of your medical education program. Develop a follow-up plan that includes customer relationship management tools to reinforce your educational content, field force follow-up materials, and deploying the content via owned media to combat the forgetting curve over time. Take your follow-up further by including audio, visual, and kinesthetic multisensory communication vehicles.
Consistent use of a follow-up strategy dramatically increases the odds that the physician will recall your information when it’s needed most.
5. Emphasize measurement
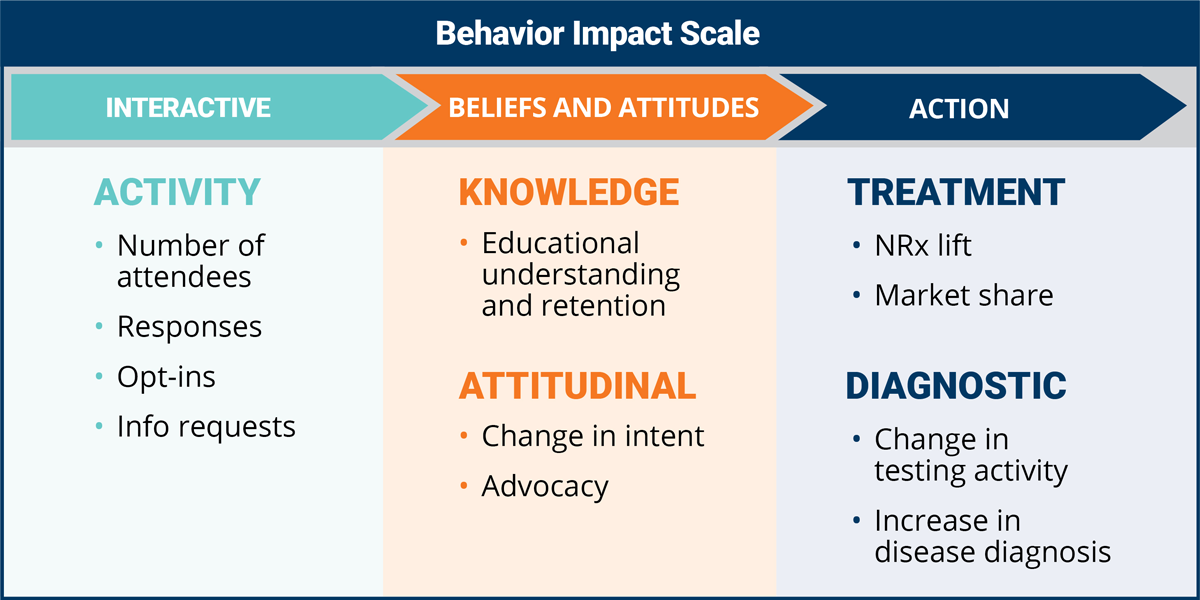
Do you measure Promo MedEd programs for performance or attendance? Typically, tactical metrics such as the number of attendees, live polling responses, and program satisfaction surveys are used. These measures provide a program snapshot and are undoubtedly important. However, they do not measure the true success of your medical education efforts when the job is to influence sentiment and intent.
Measuring progress along the entire learning journey is the most effective way to determine program success. By defining the learning journey, a chain of evidence is established for measuring program impact. Ensuring key performance indicators tied to the learning journey should be central to your measurement strategy.
Tailored to your company’s specific situation, a behavior impact scale measures discrete segments along the learning journey.
- The tactical phase measures initial program perceptions.
- The beliefs and attitudes phase measures the change of cognitive variables such as knowledge and attitude seeking to know that there’s enough understanding and retention of the program content. As the educational content is retained, attitudinal measures evaluate the change in sentiment and intent of the healthcare provider.
- The action phase measures the change in diagnostic testing and prescribing in the marketplace.
Measure for impact, not just attendance. Assessing the results of medical education programs along the learning journey provides insight into the true efficacy and influence of your educational programs. The feedback from initial impressions, effectiveness of understanding, and shifts in sentiment are invaluable to supporting physicians and their practice.
Bringing it all together
Seek and you will find many opportunities exist for enhancing your medical education programs. In today’s environment where healthcare providers are oversaturated with information, time for education is limited, and human attention spans are diminishing, it’s imperative to make every interaction matter and go beyond the one-and-done medical education program.
Performance-driven medical education is an innovative way to engage, influence, and spark behavioral change. It’s a disciplined process, not a single event, that begins with an education-first mindset that transforms the way medical education is done.



![6 Digital Tools at the Center of Healthcare Digitalization [INFOGRAPHIC]](http://ec2-54-175-84-28.compute-1.amazonaws.com/pharma-mkting.com/wp-content/uploads/2021/04/6DigitalTools_600px-218x150.jpg)



![6 Digital Tools at the Center of Healthcare Digitalization [INFOGRAPHIC]](http://ec2-54-175-84-28.compute-1.amazonaws.com/pharma-mkting.com/wp-content/uploads/2021/04/6DigitalTools_600px-100x70.jpg)




