Most physicians do not seem to know that “there is no such thing as a free lunch.” Medscape’s 2012 Ethics Report survey, for example, revealed that 72% of 23,710 physician respondents answered “Yes” to the question “Do you feel that you could be unbiased with prescribing habits if you accept lunches from pharmaceutical representatives?” (see here).
But, according to other researchers, such thinking is a “slippery slope” on which “Physicians fail to recognize their vulnerability to commercial influences due to self-serving bias, rationalization, and cognitive dissonance” (see “Physicians Under Pharma’s Influence: Are Physicians Powerless Pawns of Pharma Psychology?“).
Time and time again, when I write about physicians getting free lunches delivered by sales reps, someone always comes forward and says something like “It’s ridiculous to think that I can be influenced by a $10 lunch!”
But what if it was a $20 lunch? More recent research indicates those lunches have significant ROI in terms of prescribing brand name drugs.
Accepting a single pharmaceutical industry-sponsored meal was associated with higher rates of prescribing certain drugs to Medicare patients by physicians, with more, and costlier, meals associated with greater increases in prescribing, according to an article published online by JAMA Internal Medicine.
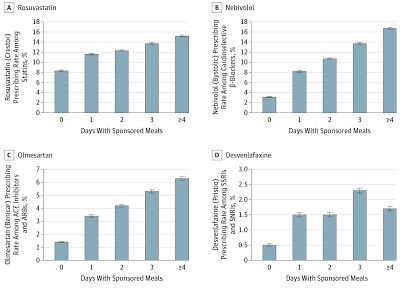
Authors identified the most-prescribed brand-name drugs in each of four categories in Medicare Part D in 2013. The target drugs were rosuvastatin calcium among statins, nebivolol among cardioselective β-blockers, olmesartan medoxomil among angiotensin receptor blockers (ACE inhibitors and ARBs), and desvenlafaxine succinate among selective serotonin and serotonin-norepinephrine reuptake inhibitors (SSRIs and SNRIs). The 2013 Open Payments database describes the value and the drug or device promoted for payments to physicians for five months in 2013 as reported by pharmaceutical companies.
Authors report 279,669 physicians received 63,524 payments associated with the four target drugs, with 95 percent of those payments being meals that had an average value of less than $20. Rosuvastatin accounted for 8.8 percent of statin prescriptions; nebivolol represented 3.3 percent of cardioselective β-blocker prescriptions; olmesartan represented 1.6 percent of ACE inhibitor and ARB prescriptions; and desvenlafaxine represented 0.6 percent of SSRI and SNRI prescriptions.
Physicians who received meals related to the targeted drugs on four or more days prescribed rosuvastatin at 1.8 times the rate of physicians receiving no target meals, nebivolol at 5.4 times the rate, olmesartan at 4.5 times the rate, and desvenlafaxine at 3.4 times the rate, according to the results. Physicians who received only a single meal promoting the four target drugs also had higher rates of prescribing those medications, the results suggest. And as the chart below shows, additional meals and costlier meals were associated with higher prescribing rates.
 |
| Click on image for an enlarged view. |








![6 Digital Tools at the Center of Healthcare Digitalization [INFOGRAPHIC]](http://ec2-54-175-84-28.compute-1.amazonaws.com/pharma-mkting.com/wp-content/uploads/2021/04/6DigitalTools_600px-100x70.jpg)